
1. Eczema
If you’ve ever experienced an eczema breakout, you are far from alone. Approximately 31.6 million Americans have eczema, according to the National Eczema Association. “Eczema is a condition that causes patches of skin to become dry, inflamed, and irritated,” explains Joel Schlessinger, MD, a board-certified dermatologist in Omaha, NE and RealSelf contributor. “It’s characterized by a dry, itchy, and sometimes scaly rash that commonly appears on the face, the backs of the knees, and the wrists.” It can also show up on the neck, ankles, or in areas that bend such as the inner elbow.
While the exact cause of eczema is unknown, it typically runs in families, particularly those with allergies, asthma, or hay fever. Many people who have eczema also have allergies to various products, such as soaps, lotions, and laundry detergents. In infants, eczema can cause an oozing or crusty rash, typically on the face, particularly the cheeks and chin. Treatment typically involves topical creams and balms. Check out these key facts about eczema and how to treat it.

2. Hand eczema
This form of eczema tends to crop up on the palms, fingertips, and finger web spaces in the form of a scaly, dry, red and cracking rash. It’s often caused by chronic repetitive insults to the skin barrier of the hands, with common culprits including irritating substances, according to the National Eczema Association. The best way to treat hand eczema is to minimize exposure to irritants and use protective gloves when doing any work that involves wet materials. “Gloves should be changed out frequently, and a cotton glove can be worn under non-breathable gloves to make them more comfortable,” says Jennifer Chen, MD, a dermatologist at Stanford Health Care in Redwood City, CA. “A heavy bland moisturizer should be used regularly such as petrolatum, or thick moisturizing cream and, in more severe cases, topical steroids, phototherapy, and even oral medications may be used to control the symptoms,” she says.
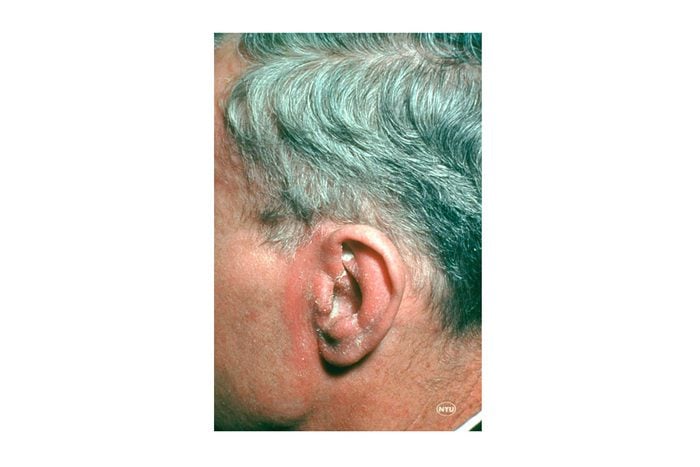
3. Seborrheic dermatitis
This scaly, itchy, red rash typically affects oil-rich areas of the body such as the face, specifically on the forehead, eyebrows, nose, and lower cheeks, as well as the ears. When infants develop seborrheic dermatitis, it’s often known as “cradle cap.” “An exact cause is still unknown, but it’s theorized to be a reaction to Malassezia yeasts that reside on human skin,” says Zain Husain, MD, a dermatologist at the Dermatology & Skin Surgery Center of Princeton in Princeton, NJ. “There are also likely genetic, environmental, hormonal, and immunologic factors that contribute to this condition,” he says. Mild cases can be treated with over-the-counter anti-dandruff shampoos and barrier repair creams, says the American Academy of Dermatology.

4. Contact dermatitis
The condition called contact dermatitis flares in response to products you’re applying to hands, chemicals, and latex gloves, per the Centers for Disease Control and Prevention (CDC). “Contact dermatitis is most often characterized by itching, scaly skin, small and large pink patches that occur in the areas that have contact with the allergen or irritant,” explains S. Manjula Jegasothy, MD, a dermatologist and founder of the Miami Skin Institute in Coral Gables, FL. “If not treated early, lesions may become infected and develop blistering, which can scar,” she says. The best way to avoid contact dermatitis is to steer clear of the trigger—if you can determine what that might be. To relieve a mild reaction, your dermatologist may prescribe a steroid cream to reduce the rash.

5. Urticaria (Hives)
These red, itchy bumps can be caused by a variety of factors including an allergy to medications, infection, insect bites, and even food. “Many cases of mild hives are common and often resolve spontaneously, however, treatment with an oral antihistamine or a topical antihistamine can ease up the resolution of the rash by as much as 70%,” says Dr. Jegasothy. “For a chronic hive that comes and goes, oral antihistamine treatment for weeks at a time may be necessary to lower histamine levels on a semi-permanent basis,” she adds. If the reaction is severe and you experience wheezing or difficulty breathing, seek medical attention immediately.

6. Psoriasis
Psoriasis is an autoimmune disorder causing the skin to become inflamed with red, thickened patches and silvery scales called “plaques.” Certain triggers can set off the autoimmune response in your body, signaling skin cells to grow too quickly. “These triggers in your lifestyle or environment might be stress, diet, allergies, certain medications, or injuries to the skin,” explains Dr. Schlessinger. “For those with psoriasis, the body cannot shed skin cells fast enough, so instead the cells pile up on the skin’s surface, causing patches of red, thickened skin with silvery scales.” See your dermatologist for the best treatment plan for you, as symptoms can affect your quality of life.

7. Heat rash
Also known as prickly heat or miliaria, this red or pink rash shows up in skin creases or areas where clothing rubs against skin and can show up in adults and babies. “Heat rash develops when sweat ducts become blocked and swell, which leads to soreness, blisters, and often itching,” says Dr. Schlessinger. “It typically begins with excessive perspiration in a hot, humid environment and is most common in infants, since well-meaning parents often dress their babies warmly no matter the climate.” The best way to treat heat rash at home is to keep the affected area cool and dry, let skin air dry after a bath or shower, and avoid any tight clothing, says the Mayo Clinic.

8. Rosacea
With rosacea, the skin tends to appear red or flushed, almost like you’re blushing. Although the exact cause of rosacea is unknown, there are factors that can worsen its symptoms. “Facial redness can become worse with sun exposure, wind, colder weather, hot beverages, alcohol, spicy foods, stress, and exercise,” says Dr. Schlessinger. “In some patients, rosacea is caused by a bacteria called H. pylori, the same bacteria that cause ulcers in your stomach, as well as skin mites.”
Your dermatologist may recommend prescription medication and IPL (Intense Pulsed Light) treatments. “IPL treatments gently deliver precise amounts of intense pulsed light through the skin’s surface to treat rosacea on the face, neck, and chest,” explains Dr. Schlessinger. “They might also recommend over-the-counter skincare products that are gentle enough for sensitive skin.”
While there’s no way to completely prevent rosacea, simple lifestyle changes can help diminish the symptoms, such as avoiding extreme temperatures, wearing sunscreen at all times, turning down the heat, avoiding certain rosacea food triggers, and running a humidifier at home.

9. Shingles
The painful skin rash of shingles appears in a strip that wraps around one side of the body and is most common in older adults and those with weak immune systems. “It’s caused by the reactivation of the varicella-zoster virus, the same virus that causes chickenpox,” says Dr. Husain. “The virus remains dormant in nerves until reactivated,” he says.
Approximately one in three adults will get shingles in their lifetime, most likely after age 50. “Before the rash appears, you may have a headache or flu-like symptoms, followed by itching, tingling, or pain and after the rash appears, it may turn into a cluster of blisters, which can take several weeks to heal,” says Dr. Schlessinger. Treatment involves antiviral and pain medications that are most effective when started early, as they can help the rash heal faster and minimize pain.

10. Intertrigo
This rash shows up in moist folds of skin, like the neck, armpit, groin, and between fingers, from the constant rubbing of skin surfaces. It’s often associated with bacterial, fungal, and viral skin infections. Symptoms include redness, sensitivity, pain, and oozing. Treatment is often directed at keeping the affected areas dry with medicated powders, barrier creams, and antiperspirants. Since it’s often associated with excess weight, losing weight may be helpful, as is keeping body folds dry.

11. Swimmer’s itch
Ever finish a long day at the beach or pool and notice itchy, raised red bumps? This is known as swimmer’s itch, a common allergic reaction to parasites found in and around water sites. While the parasites prefer their intended target—birds and mammals—they’re also known to burrow into human skin. “Symptoms include itching or burning sensations on the skin and pimples and blisters that show up several hours after being in non-chlorine treated water, oceans or brackish water,” says Dr. Jegasothy. “The rash will usually go away on its own in about a week without treatment. However, if it persists or there are signs of infection such as increased warmth, redness or pain, red streaks, pus, and fever, see your doctor immediately.”
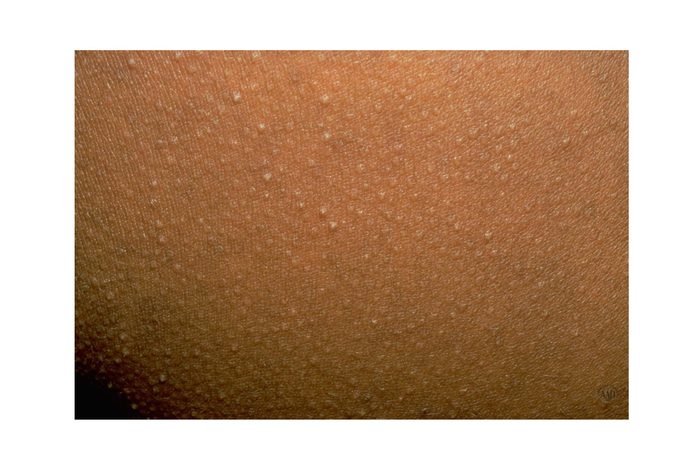
12. Keratosis pilaris
Also known as “chicken skin,” keratosis pilaris is characterized by tiny, rough, skin-colored or red bumps around hair follicles on the upper arms, thighs, buttocks, and occasionally the cheeks. It’s caused by a genetic predisposition to a buildup of keratin plugs on the skin that results in clogged hair follicles. “Over-the-counter topical steroid cream can help, followed by a moisturizer containing glycolic acid, which dissolves the keratin bumps clogging the pore,” Dr. Jegasothy explains.”It’s best applied when your skin is warm and most, such as immediately after the shower,” she says. If OTC treatment is ineffective, or if there’s more redness accompanied by tenderness and swelling, schedule a visit with your dermatologist.

13. Cold sores
Those nasty cold sores are characterized by small red, swollen blisters that develop on the lips and around the mouth and may stick around for up to two weeks, according to the AAD. “Cold sores are caused by the herpes simplex virus, which is easily spread through contact with someone who is infected, including by sharing drinks, razors, and other personal items, as well as kissing,” says Dr. Schlessinger. Your dermatologist can diagnose a cold sore through a simple examination and recommend over-the-counter topical treatments to help relieve painful or irritating symptoms.

14. Pityriasis rosea
The skin disease pityriasis rosea is characterized by rashy dry patches. It often starts out with one “mother patch,” followed by smaller “daughter patches.” The exact cause is currently unknown, though one thought is that it originates from a virus. “Pityriasis rosea usually goes away without treatment in anywhere from two to eight weeks,” says Dr. Jegasothy. “Cortisone or antihistamine treatments are available for unbearable itching,” she says.
