Dozens of My Friends Have Had Coronavirus—Here’s What They Want You to Know
Updated: Sep. 01, 2023

One by one, I've watched friends and family members contract, spread, and battle coronavirus. They've shared their stories in the hope of helping others.
While it’s true that the ever-growing coronavirus pandemic seems to be most deadly for older adults and those with underlying health conditions, anyone can contract it, exhibit serious symptoms, and spread it to others. Even with all of the new social-distancing norms and cultural shifts, no age group or demographic is immune to the virus. I learned that the hard way when my own friend died from coronavirus complications early in the pandemic. He wasn’t who you might expect—he was a bright, funny 34-year-old man with a normal, vibrant life and a mild history of childhood asthma and bronchitis. Jeff’s death in March 2020 was just the beginning of a cascading series of COVID-19 cases in my expanded network of friends and family, with loved ones catching the virus at small gatherings, work, and various unexpected places. By December 2020, I was able to count more than 20 friends and colleagues under the age of 45 who had passed away from coronavirus complications, none of whom had any major or unusual health issues prior to contracting the virus.
We know so much more about COVID-19 and how it spreads than we did last spring, but some people still believe the virus is a hoax when it most certainly isn’t. Even with millions of people being vaccinated each day, it continues to harm so many people, which is why these stories from my friends, colleagues, and family members across the country who have contracted coronavirus are so important. Here’s what they want you to know.
You can do everything right and still catch the virus
“I contracted COVID in my own home,” says Eliyanna Kaiser, a 41-year-old mother from New York City. “My child can’t go without his autism therapies, and a therapist who comes to our home regularly gave it to us when she didn’t realize she was infected. She was asymptomatic.” While having a therapist come and go from her home may seem like an obvious red flag, Eliyanna explains that she took all of the recommended precautions. “We wore masks, kept as much distance as possible, and left the windows open, but it didn’t matter,” she says. “When someone close to the therapist developed symptoms, she got a test and alerted us.”
Eliyanna came down with a fairly serious case of COVID-19, and the symptoms have persisted like a weeks-long roller coaster. “I thought I was on the road to recovery and just dealing with lingering exhaustion when I had the biggest scare of all,” she says. “My heart was pounding and fast, like I had been running for my life, except that I was lying on the couch, relaxing, and watching movie. I grabbed my pulse oximeter and saw that my heart rate was 147. After several hours, it was still in the mid 140s and I realized that I needed help, so I called my doctor and was told to go to the emergency room.” Because her doctor was worried she might have a stroke or heart attack, and she didn’t want to expose a taxi driver to COVID, she asked a friend to walk the 15 blocks to the hospital with her.
She was subsequently diagnosed with tachycardia, an inflammation of the heart tissue that’s common with COVID. “Weeks later, I still have an elevated heart rate compared to before, but nothing as scary as 147,” she says. “Time will tell if there is some kind of permanent heart issue. I hope not.” Why do some people get so sick from COVID and others don’t? It’s one of the coronavirus mysteries that still can’t be explained.

Mild cases can become incredibly serious, even months later
My friend Tara is no longer here to tell her story because she died right after Christmas, her favorite holiday, at only 30 years old. She actually got COVID-19 in May from her job in sales. She wore a mask religiously, and after she got a positive test, she isolated in her studio apartment by herself. We texted daily, FaceTimed, and shared phone calls through her two-week recovery. Her symptoms were fairly mild. She had a persistent fever for the first 10 days or so, a lot of coughing, and a headache that I remember her saying felt like it was “piercing” her skull. But then she got better and was back to life, albeit more cautiously, and as vibrant as ever.
In December, though, I got a phone call from one of our mutual friends. Tara, the healthy, exciting, life-of-the-party smile machine, died suddenly of a heart attack. It didn’t make sense. She was only 30, loved yoga, paddleboarding, long walks, and being active. Apparently, Tara’s COVID was relatively minor in outward symptoms, but it had left massive scar tissue on her heart. Her team of specialists at Mount Sinai Hospital in New York who examined her after her death said she was a “ticking time bomb.”
Tara spent the last several months of her life posting “Mask Up!” memes on social media, encouraging her friends and family abroad to take the virus seriously, and asking her workplace to enforce COVID-19 safety measures. But it wasn’t enough to prevent her untimely death.
You can still get it after your first round of the vaccine
“I received the first vaccine right before I got sick,” says Judith, an otherwise healthy 38-year-old woman who recently moved to Israel from California. She received the Pfizer vaccine on January 16, but just a few days later, her whole immediate family tested positive for the virus. Of course, the vaccine requires two doses, spaced out several weeks apart; medical professionals caution that you do not have immunity until two weeks after the second shot. Unfortunately, Judith’s husband caught COVID from a colleague and spread it to her and the rest of the family before the vaccine had a chance to work.
What first started as brain fog for her turned into severe headaches, fever, and extreme fatigue. “I physically could not lift my head off the pillow for a week and took Tylenol around the clock,” she says. “At nearly three weeks, I still have lingering fatigue but otherwise feel much better. This virus was truly unlike anything I’ve ever experienced. It felt worse than the flu and lasted much longer, and it was like it took over my entire body from my brain down to my toes.”
While the rollout of the vaccine has spurred hope and visions of getting back to normal, we still have a long way to go. And as Judith’s story clearly illustrates, this isn’t the time to get back to life as we knew it before the pandemic, says Jonathan Baktari, MD, a pulmonary and critical internal medicine doctor and the CEO of e7 Health. He suspects the average American won’t have easy access to either of the vaccine options until the second half of 2021. “I would say early fall we should be pretty good,” he surmises. “The last holdup is we don’t have vaccines for children, and they haven’t been studied, especially in the population below 12 years. Vaccines for the population below 12 are probably not going to be available [before] fall.” If you qualify now, here’s how you can get the COVID-19 vaccine at Walmart.
The virus tricks you into thinking you’re OK
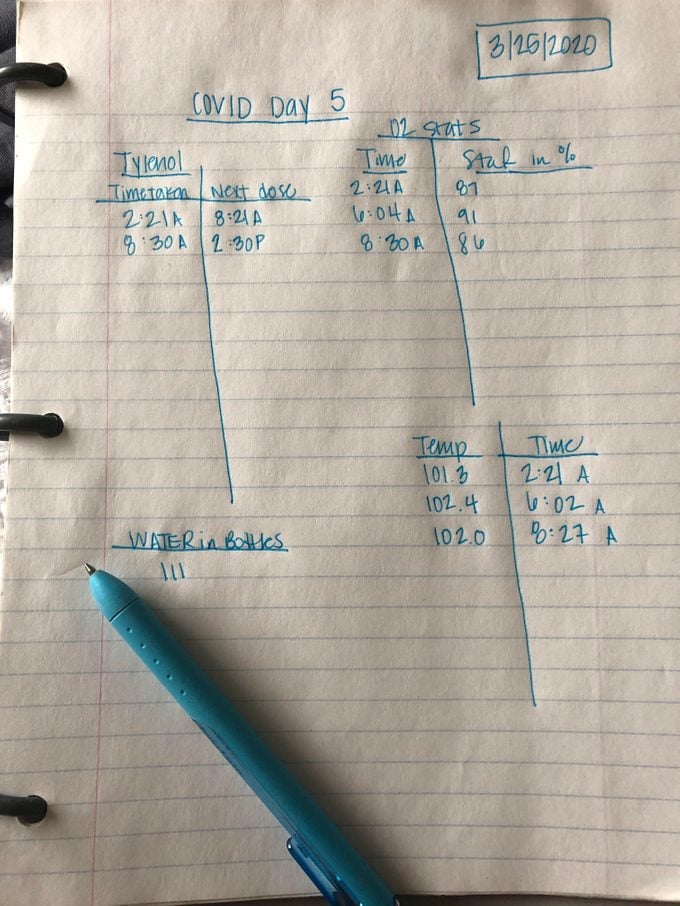
While some people can’t pinpoint their source of contagion, others know exactly who gave them coronavirus. Jenny Cotie Kangas, a 33-year-old from Apple Valley, Minnesota, believes she contracted COVID-19 from a coworker. At the time, she couldn’t get a test because Minnesota was only giving them to those who were critically ill, but she was presumed positive and monitored her symptoms at home. “I checked my own oxygen stats and recorded them along with my temperature every day. In the event that I had to go to the hospital, I would be able to share this information with them, but [it also helped me] recognize when my symptoms were changing,” she says. “The virus is a roller coaster, and it tricks you into thinking you’re better when you aren’t.”
Jenny, who is a single mother, had her kids stay with her ex-husband as she recovered. She understood the importance of isolation and steering clear of others, given the extremely contagious nature of COVID-19. While battling this illness was tough, she remained grateful for her support system. “I had family calling to check on me. I have an ex-husband who was dropping off cooked meals at my door since I was too weak to cook—and he had my three kids while I was sick,” she says. “I’m scared for the people who don’t have that support. Just being on your own for this long is hard, let alone being sick.”
Jenny was lucky her symptoms were relatively mild and she was able to recover quietly at home. Still, it took several weeks for her to feel back to normal.
It’s more contagious than you can imagine
“People do not understand how contagious this is,” shares Jacquie Rosshandler, who lives in New York. The 38-year-old entrepreneur and mother of two attended a charity dinner last March, which is where she contracted the virus. “My husband and I made a promise to ourselves not to touch anyone, thinking this would protect us. In fact, we promised to go into isolation, and this was going to be our last social event,” she says. “It also happened to be the social event that did us in.”
This was, of course, before we knew about the importance of mask wearing, social distancing, and proper ventilation. Jacquie, her husband, and several other guests fell seriously ill and tested positive for coronavirus. During the incubation period, those infected at the event continued to move about New York, and some even traveled internationally.
The sickness was brutal for her family. “We are both very athletic, eat well, don’t eat meat, and are in very good health,” she explains. “[But] the headaches for me lasted four days and were quite painful. Tylenol didn’t help at all.” Her husband suffered severe fever and sweating episodes, and was still sweating through clothes and bed sheets regularly after 10 days.
Jacquie hopes that more people will be proactive about preventing additional spread by canceling plans for gatherings of all types and not mixing households. “Isolate yourself for the good of yourself and the entire community,” she says. “Stop waiting for other people to tell you to do so.” In case you were wondering, declining or changing your RSVP is perfectly fine right now.
Don’t expect fast test results
If you’re hearing about fast-result coronavirus tests and thinking you’ll have access to one, that just may not be the case. Plus, the PCR tests are more accurate than the rapid ones, and they take between two and five days to get results back. Stephanie S., from Wycoff, New Jersey, waited six full days to finally receive word that her coronavirus test was, in fact, positive. The 35-year-old’s husband, who wasn’t tested, also began exhibiting strong symptoms. They’re not sure how or when they contracted the virus.
“This virus is crazy,” she says. “Just when you think you are feeling 100 percent, it takes a turn for the worse and hits you with more chills, exhaustion, and fever—all while you’re dealing with an intense cough that makes your chest hurt. It started with my chest feeling tight like I had a cough coming on, and then I came down with a mild fever accompanied by body aches and chills, and extreme exhaustion and a very bad cough.”
It took several months for Stephanie to feel completely recovered, but she now worries about the unseen long-term damage the virus might have done. Unfortunately, she adds, few doctors are proactively running tests to check for serious damage or complications beyond what the naked eye might find.

The sickness takes an emotional toll, as well
Early in the pandemic, Josh Berg of Woodbury, New York, had trouble getting a test. After experiencing a three-day fever that was consistently around 102.5, his doctors told him to just assume he had it. He eventually managed to get a test at a nearby urgent care and was, indeed, positive for COVID. His wife never got a test, but she experienced the same symptoms and more—including a complete loss of taste and smell, one hallmark symptom of coronavirus everyone should know about. They also both experienced muscle aches, acute breathing issues, and fever.
The virus took a toll on them, both physically and emotionally. “I don’t have a negative bone or depressed ounce in my body, but it definitely starts to wear on you,” Berg says of the symptoms and resulting isolation. “Anger, frustration, depression, helplessness. It’s all present.”
The exhaustion is “paralyzing”
“The first symptoms I felt came all at the same minute,” says Monique P., a 35-year-old mother from Brooklyn, New York. “I was practically paralyzed with exhaustion, and I had a fever and sore throat. My first thought was: I feel like I was hit by a train. My doctor didn’t believe it was coronavirus. I was tested for strep and the flu, but both swabs came back negative.”
Her 101.5-degree fever persisted, and on day three, she started experiencing pain behind her eyes and in her sinuses. The following day, Monique took a coronavirus test, and by then, she had lost her senses of smell and taste. On day five, she developed heart palpitations, tingling skin, the feeling of something crawling on her, a burning sensation in her nose, and a cough. On day 11, she was still weak, fatigued, and only able to taste salt. It took more than a month for her to feel like herself again, and even longer for all the symptoms to fully subside.
She’s optimistic, though, about how society will change once this pandemic has passed. “I think people will be kinder from this,” she says. “You can’t go through a trauma and come out the same.” These uplifting stories of neighbors helping during coronavirus will inspire you to do the same.
Early symptoms are often gastrointestinal
Chayim B. Alevsky, a 52-year-old rabbi from Manhattan, couldn’t imagine that he and his 10-year-old daughter had contracted coronavirus when they began vomiting after intense nausea that lasted several days. But that’s exactly what had happened. The nausea led to sweating episodes so severe that multiple layers of clothes were left drenched. “My daughter noted a feeling of tightness in her chest, but neither of us had a sore throat or cough,” he says, although the stomach-related symptoms of nausea, vomiting, diarrhea, and food aversions persisted somewhat severely.
Despite their ordeal, he’s looking toward the future with hope. “We see that something almost invisible—a virus—can affect the world with such speed, and I’m hoping we can use that concept to spread kindness at the same rate,” he says.
Even young, healthy people with no preexisting conditions can become long-haulers

Nadia Ackerman, an artist from New York better known as “Natchi,” caught COVID at the same event that Jacquie Rosshandler attended last spring. “It felt like someone was punching me on the inside—like I had been kicked by a horse,” the 45-year-old says of her coughing attacks, ongoing fever, scratchy sore throat, extreme malaise, and exhaustion, which was then followed by nausea and a loss of taste and smell. “I spent four days in bed thinking it would pass soon. Everyone was telling me I was young and strong and I’ll be fine. I wasn’t fine. On the fifth day, I woke up to take a sip of water that was immediately met by vomiting and diarrhea. I called 911 and an ambulance took me to the emergency room, where I was treated for severe dehydration, nausea, and headache as a result of the coronavirus.”
It took nearly six months for Natchi’s senses of taste and smell to return, and then it was replaced by a phantom smell of cigarette smoke—all the time, whenever she was indoors. She thought she was going insane. Also, in July, nearly four months after her initial infection, she woke up in the middle of the night with severe stomach pains. She thought she was going to die on the spot. The pain was accompanied by sudden fever, vomiting, sweating, and labored breathing. When she went to the emergency room the next day, the doctors took some X-rays and found that she had COVID lungs.
Natchi’s diagnosis landed her in the hospital for a second time. “I had thickening of the bronchial walls, and they also found a pulmonary embolism in my lung,” she says. “They gave me blood-thinner injections and admitted me to the ward. They said there was a lot of inflammation throughout my body. After that hospital visit, I just wasn’t myself. I was extremely lethargic. Everything I did seemed difficult. I also developed a strange sore on the bottom of my leg the size of a quarter that would not heal. It turned out to be nummular eczema. That’s another thing I have never had in my life that was brought on by my COVID infection.” Nearly a year later, she is still dealing with long-hauler symptoms.
She wants people to know that even the healthiest 45-year-old person—someone who does yoga, leads a vegan lifestyle, and has no preexisting health conditions—can easily contract and suffer from coronavirus. And she’s worried that people are letting down their guard. “The thing about this virus is that it comes and goes in waves,” she explains. “Stay home—not only for [yourself] but for other people.”
You can get it again
When Darren P. from Florida found himself shaking with an ongoing low-grade fever a few weeks ago, he wondered if he’d gotten the flu. “I had COVID back in June. A lot of people in my area in Florida had it then, and I didn’t get it too bad the first time,” he says. “I stayed home for a couple of weeks mostly out of concern for others, but I really just had a cough and some exhaustion. I believed if I had it once, that it would be like the chickenpox—never again. Boy was I wrong.”
By January, Darren had grown laxer about precautions. When he started experiencing nausea, a low-grade fever, and brain fog he called his doctor. “My doctor said more and more people around Miami were getting COVID a second time, especially with all the mutations. I didn’t know that my antibodies were only temporary in the scheme of things, and I wish I understood that earlier because the second time feels much more intense than my first go of it.”
You’ve probably heard about the U.K. and South African coronavirus mutations, and there’s a reason they’re of particular concern. “While the vast majority of mutations have little import, a single mutation that makes the virus more dangerous can rapidly make this terrible pandemic even more deadly,” explains Richard Pan, MD, a California state senator, national expert on vaccination policy, and chair of the California Senate Committee on Health. “We have given the coronavirus over 22 million opportunities to mutate so far. We must increase efforts to reduce the further spread of the virus by enforcing universal mask wearing, halting non-essential gatherings of people living in different households, and isolating and quarantining all infected and exposed people to prevent to the emergence of more serious viral mutations.”

Anxiety may exacerbate your symptoms
Even if your symptoms aren’t severe, you still need to take them seriously. Taylor B., a 32-year-old who lives in New York, had only mild symptoms for about two weeks. However, her experience wasn’t a walk in the park. “The shortness of breath was scary—and trying to calm myself down while living in a small studio apartment was a real challenge some days,” she says. Her anxiety persisted for several weeks.
Shortness of breath is common for even the mildest COVID-19 cases, but it may also be due in part to the extreme anxiety so many people are facing now. In fact, roughly 20 percent of people who have contracted the coronavirus ended up battling some form of depression, anxiety, dementia, or other psychiatric disorders. Some of these issues can also have a delayed onset; according to some reports, they may not show up for three months. All that said, if you’ve tested positive and are experiencing shortness of breath, you should speak to your doctor immediately.
You’ll need to fight
Jason Hasty, a 54-year-old attorney from Augusta, Georgia, openly chronicled his own coronavirus journey because of his public candidacy for district attorney. On day 11 of his quarantine, his symptoms were still going strong. The World Health Organization says recovery typically takes three to six weeks, and one study found that the majority of those who contract COVID-19 and are at least 30 years old take several weeks to recover, even if they have mild cases.
“I woke up this morning alone again,” Jason posted on social media on day 11. “The first thought was where am I? What day is it? And then that heavy, restricted feeling hit me in my chest, and then I remembered. I remembered what my new normal is. Staring at these four walls in my quarantined bedroom.”
His posts, which garnered a lot of local attention, offered a stark look into the emotional ups and downs of the coronavirus, as well as the physical toll it takes. And he has an important message for anyone who finds themselves in this situation: “You just fight. You get up every day and you take your medicine and your vitamins and you pray you are going to make it. You start screaming from the mountaintops to save anyone you can. Don’t just go home to die. Fight. You have to fight to get well. You have to beg for health care. You have to plead and argue. This is no time to be nice and timid.”
Jason eventually recovered, but it took a full six weeks for him to feel like his usual self and he still experiences muscle aches nearly a year after his initial infection. The pandemic may alter your outlook on life—it did for these people who changed their bucket lists because of it.
For more information on COVID-19, see our comprehensive Coronavirus Guide.
Sources:
- Jonathan Baktari, MD, a pulmonary and critical internal medicine doctor and the CEO of e7 Health
- Nadia Ackerman, an artist better known as “Natchi“
- Richard Pan, a California state senator, national expert on vaccination policy, and chair of the California Senate Committee on Health
- Healthline: “People with COVID-19 More Likely to Develop Depression, Anxiety, and Dementia”
- The Lancet: “Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA”
- Journal of Infection: “Effects of age and sex on recovery from COVID-19: Analysis of 5769 Israeli patients”