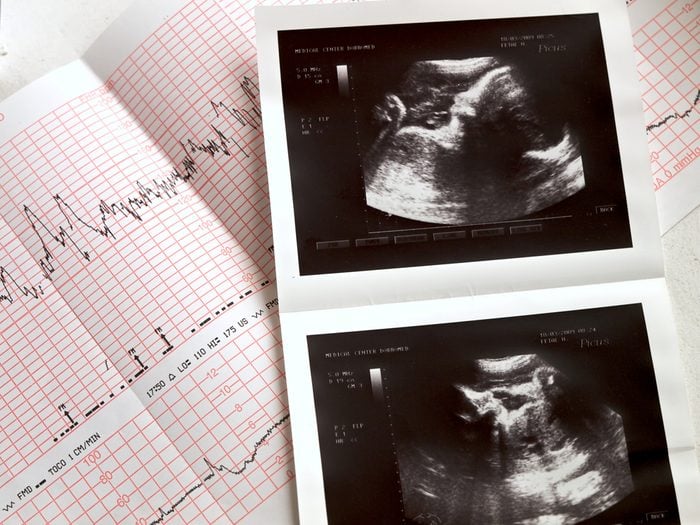
Pregnancy
Some women will experience abdominal pain after sex during pregnancy—so if you’re experiencing it, you’ll first want to rule out pregnancy. “An ultrasound can confirm the pregnancy, and determine if the abdominal pain is due to an ectopic pregnancy; that’s when the fertilized ovum implants outside of the uterus. Another possibility is a miscarriage before 20 weeks,” says Risa Klein, CNM, certified nurse midwife. It’s easy to miss these very early pregnancy symptoms.

Endometriosis
One of the common signs of endometriosis—which strikes about 1 in 10 women of childbearing age—is abdominal pain after sex. In women suffering from endometriosis, cells resembling those of the uterus starts growing in other parts of the body, including the fallopian tube, explains Klein. Other symptoms of endo can include painful periods as well as infertility. If you think you might have endometriosis, find a doctor who is an expert in endometriosis treatment and management, recommends Aimee Eyvazzadeh, MD, San Francisco-based fertility specialist. Here are facts no one tells you about endometriosis.

Adenomyosis
This condition, which is closely related to endometriosis, triggers pain due to uterine glands growing into the muscle wall; the glands can grow and bleed with a cycle of their own, explains Felice Gersh, MD, OB/GYN, founder and director of the Integrative Medical Group of Irvine in California and author of PCOS SOS. “With sexual relations, sufferers can experience cramping or aching,” she says. “While there is no cure for adenomyosis, a hysterectomy (if fertility is no longer an issue), oral contraceptives, and other contraceptives designed to alter hormones may provide relief from symptoms,” she explains. Are you on the wrong type of birth control?

A malpositioned IUD
An IUD (intrauterine contraceptive device) that becomes partially or fully displaced from the top of the uterine wall could create abdominal pain after sex, according to Klein. “This can feel like a pressure or poking pain. It could settle into another area of the uterine wall or in your cervix—and that could also cause pain,” she says. “A vaginal exam or ultrasound could determine the location of the IUD; if it is dislodged, the IUD would need to be removed by the provider.” Here are reasons you might switch from birth control pills to the IUD.

Uterine fibroids
Also called leiomyomas or myomas, these tumors of the uterus, if they’re large enough, can cause significant pain during intercourse, according to Mark Trolice, MD, reproductive endocrinology and infertility specialist at My Fertility CARE: The IVF Center in Winter Park, FL. “These are benign tumors of the uterus that can grow inside the uterine cavity (submucous), in the muscle (intramural), under the outer surface (subserosal) or attached to the outside (pedunculated) and have no known cause,” he says. Treatment can include over-the-counter pain relief, such as ibuprofen, birth control pills, or surgery to remove only the fibroid or uterus. Learn to recognize the silent signs you have uterine fibroids.

Pelvic floor hypertonia
This condition occurs when the muscles in the vagina become tight and contract, making intercourse painful. “The muscles and nerves can begin to deteriorate and become tender and overactive, causing more pain,” says Terry Dunn, MD, owner of Foothills Urogynecology. “Symptoms include incontinence, pelvic tilt, hip instability, weak core muscles, and lack of upper-body strength.” Relaxation techniques, mind-body medicine, and cognitive behavioral therapy can be helpful in treating this condition; stress often plays a role in the development of pelvic floor pain, according to Dr. Gersh. Are you at risk for pelvic-floor dysfunction?

Pelvic inflammatory disease
If you experience a new pain in your lower abdomen and pelvis, an unpleasant vaginal odor, and pain or bleeding during intercourse, you should be tested for this inflammatory condition—it hits an estimated 88,000 American women between the ages of 15 and 44, according to the U.S.Department of Health & Human Services. “Sex may worsen the condition and cause a dull pain in the lower belly,” says Nicole Williams, MD, a gynecologic surgeon and founder of The Gynecology Institute of Chicago, IL. “See your healthcare provider immediately if you’re suffering from this sharp pain, as it usually does not resolve on its own and requires antibiotics as a course of treatment.”

Ovarian cysts
Many women experience ovarian cysts, fluid-filled sacs in the ovary, without symptoms, and, in most cases, they’re totally harmless. For some sufferers, however, they can be quite painful. “Symptoms can include abdominal bloating or swelling, painful bowel movements, pelvic pain before or during the menstrual cycle, painful intercourse, pain in the lower back or thighs, nausea and vomiting, severe or sharp pelvic pain, or faintness or dizziness,” says Dr. Dunn. “Only 8 percent of premenopausal women develop large cysts that actually require treatment, but you should still see your doctor if you’re experiencing pressure, bloating, swelling, or pain in the lower abdomen.” Learn to detect signs of polycystic ovarian syndrome (PCOS).

Urinary tract infection
Commonly referred to as a UTI, this usually harmless bladder infection can cause burning, stinging, or midline abdominal pain before, during, and after sex. It’s an especially common occurrence after intercourse for those prone to the infection or those who’ve recently had intercourse multiple times in a row, according to Kameelah Phillips, MD, OB/GYN in New York City. “You should go to the doctor soon after these symptoms appear and be treated with a course of antibiotics to prevent the infection from worsening and traveling to the kidneys,” she says. Here is a simple solution for preventing recurring UTIs.

Dyspareunia
Recurrent or persistent pain with sexual intercourse, known as dyspareunia, typically occurs at the vaginal opening or deep in the pelvis and can be caused by numerous factors—physical, psychological, and social, explains Kristina Tocce, resident physician at Vibrant, which is a sex toy retail site started by Planned Parenthood of the Rocky Mountains. It’s possible you could identify the pain as coming from the abdomen. “Working with your health care provider to understand the location, nature, and duration of the pain is important to identify the cause or causes,” she says. Experts recommend always taking these sex problems seriously.

Deep penetration
Sometimes the cause of abdominal pain after sex is nothing more than deep penetration. “When the cervix and uterus are bumped repetitively during sex, the shock spreads through the surrounding pelvic ligaments,” explains Dr. Phillips. “It should go away on its own or with an over-the-counter medication, as it rarely requires a visit to the doctor.” Modifying the depth of penetration during sex should minimize future discomfort. Here’s how to make sex great again.

Vulvodynia
Outer vaginal pain that worsens upon penetration is often the cause of vulvodynia, a persistent vulvar pain that is present for at least three months. In some cases, pelvic pain can be clearly traced to bands of internal scar tissue (adhesions) that form after injury or infection in the pelvic or abdominal region, says menopause.org. “Though the cause is unknown, women with residual vulvodynia typically begin with behavior modification to reduce exacerbating factors and improve stress reduction,” says Dr. Trolice. “After behavior therapy, doctors may try a multidisciplinary approach that includes pelvic floor physical therapy, exercise, lubrication, warm baths, and counseling.” Antidepressants can sometimes help but no, that doesn’t mean your vagina is depressed.

Vaginal lacerations or tearing
Vaginal lacerations or tearing, often caused by sex itself, can be also be a cause of pain after intercourse. To prevent this kind of injury, use lubrication whenever dryness is present and also when using toys, says Dr. Phillips. How do you know if you have vaginal lacerations? “The nerves in the vaginal wall radiate to the lower abdomen, but bleeding is also present,” she says. “Active, bright red bleeding and nausea should send you to the ER for evaluation to make sure stitches aren’t needed.” Here are 13 things your vagina wants to tell you.
