What is glucose?
Glucose is also known as blood sugar. After eating carbs, your body breaks them down into a type of simple sugar called glucose that is then either stored or used for energy—and that’s just the tip of the iceberg. Here’s everything you need to know about glucose, even if you don’t have diabetes.

Blood sugar should be relatively low and steady
High blood glucose can be toxic and is a sign of prediabetes, so it’s crucial to keep it in check. According to the Centers for Disease Control and Prevention (CDC), more than one out of three Americans have prediabetes, and many don’t know it because it causes few symptoms (or none at all). So what is prediabetes? Typically when you eat food, blood sugar starts to rise so your body starts to produce the hormone insulin. Insulin normally lowers blood sugar levels because it signals the body cells to absorb the glucose and use it as fuel.
However, with prediabetes (which can eventually progress to type 2 diabetes), the body can ignore the effects of insulin, which is known as insulin resistance. That means that even though there’s insulin in the bloodstream, blood sugar levels remain too high, which can increase the risk of heart disease, stroke, and other health problems. (Here’s more on keeping your prediabetes from turning into Type 2.)
That’s why everyone can benefit from learning about blood glucose and how to avoid having levels that are too high. You can take steps (like exercise) that help reduce the risk of insulin resistance (and follow these tips on maintaining stable blood sugar levels).
So what should your blood glucose level be? The American Diabetes Association says that a fasting glucose level of less than 100 mg/dl is normal, with 100 to 125 as prediabetes, and over 126 as diabetes. (A fasting glucose test is a blood test conducted after you haven’t had any food or drink, except water, for eight hours.) Your hemoglobin A1C level—which is a blood test that detects levels in the previous two to three months—should be less than 5.7 percent.

Food is turned into glucose
It can be helpful to understand what exactly glucose is. “When you eat food, your body needs to convert it into the simplest form of energy, which is glucose, to utilize it,” says Erin Palinski-Wade, RD, certified diabetes educator (CDE), and author of 2-Day Diabetes Diet. “Carbohydrates are the easiest food to convert into glucose, which is why they have the greatest impact on blood glucose levels.” When we eat carbs, they’re broken down into glucose as they’re digested. Then, “glucose is absorbed by the cells lining the small intestine, into the bloodstream and delivered throughout the body,” explains Tanya Zuckerbrot, MS, RD, a New York City-based registered dietitian, bestselling author, and founder of The F-Factor Diet.

Simple carbs can make glucose spike
In general, carbohydrates are some of the healthiest foods you can eat, including legumes, fruit, and whole grains, but it’s best to go easy on the “simple” or refined carbs like sugar-sweetened beverages, white bread, pasta, cakes, and other sweets. “The amount of carbohydrate consumed at one time and the type of carbohydrate—complex or simple—will have a great impact on glucose levels,” Palinski-Wade says. (Here’s how to reverse the effects of a sugar binge.)
Zuckerbrot says to remember portion sizes when eating carbs. “One-third cup of rice, half a cup of pasta, and half a cup of lentils all equal 15g of carbohydrates or one serving of carbohydrates,” she says. “Keep that in mind when portioning out your lunch or dinner. Most restaurants give you double or triple the amount you should be eating in one sitting.”

Fiber helps keep blood sugar steady
Fiber is what makes complex carbohydrates complex—it’s the zero-calorie, non-digestible part of a carbohydrate that adds bulk to food and swells in the stomach when eaten. Studies have shown eating a diet rich in fiber can help control blood sugar. “Choosing high fiber, complex carbohydrates will slow down how quickly food is converted into glucose, which will help to stabilize glucose levels,” Palinski-Wade says. Whole grains, fruits, nuts, legumes, and other vegetables are high in fiber. In addition, check where the foods you eat fall on the glycemic index and its glycemic load, which rate how quickly the food produces glucose as well as how many carbs it contains.

Insulin resistance can cause blood sugar to be too high
“Blood glucose levels are controlled by two pancreatic hormones: insulin and glucagon,” Zuckerbrot says. The pancreas makes insulin to help the body absorb glucose (we’ll get to glucagon later). “The pancreas secretes insulin at low levels in between meals and while we sleep,” says Idie Clement, RN, certified diabetes educator (CDE) of Piedmont Atlanta’s Diabetes Resource Center. “When we eat, insulin is secreted quickly and takes the sugar from the blood stream so it can create energy and keep the blood sugars in normal range.”
Basically, insulin helps the body absorb glucose. But with prediabetes and type 2 diabetes, the body’s insulin resistance leads to a buildup of glucose in the blood. People with type 2 diabetes can combat insulin resistance and control their blood sugar with a combination of diet, exercise, oral medication, and sometimes injecting additional insulin. People with type 1 diabetes, however, always need to take insulin to survive because it’s an autoimmune condition that destroys the insulin-producing cells in the body. (Here are the differences between type 1 and type 2 diabetes.)

Glucose fuels the brain
Although glucose so far sounds like a bad thing, you wouldn’t be able to survive without it. In fact, one of the amazing facts about your brain is that your noggin runs on glucose. According to Harvard University’s Neuroscience Institute, the brain uses the most energy out of all the body’s organs, and so requires half of the body’s sugar. In addition, “glucose is the primary source of energy used by our bodies,” Zuckerbrot says. Once your body has used the energy it needs, “glucose is stored as glycogen in the liver and muscles,” she says. If your body runs low on glucose, the pancreas will release its other hormone, glucagon. “Glucagon induces the liver to release stored glucose into the bloodstream,” Zuckerbrot says.

Not eating is not good for glucose
You might ask, will skipping breakfast help lower blood sugar? It turns out that not eating is not an effective strategy for keeping glucose in check. “Spacing carbohydrate intake throughout the day to prevent consuming excessive amounts at one time is the best way to ensure steady blood glucose levels,” Palinski-Wade says. A stable blood sugar level means not having spikes or huge drops—plus, low levels might make you overeat or eat unhealthily. “Low blood glucose levels can make it harder to concentrate, make you cranky, and lead to excess snacking or cravings,” Zuckerbrot says. “Keeping your blood sugar stable throughout the day can help you avoid side effects of low blood sugar. Avoid skipping meals, and eat every four to five hours.”

Super-low blood sugar is dangerous
Every person who has diabetes should know these tricks to treat low blood sugar—but what about everyone else? Turns out that although it’s more common in people who are taking insulin to treat diabetes, anyone can become hypoglycemic, which means having dangerously low blood sugar levels. If an otherwise-healthy person develops system, it is likely because they have prediabetes and should see their doctor.
“Symptoms of hypoglycemia include feeling shaky, breaking out into a sweat, feeling your heart rate race or face flush, hunger, and sometimes, if low enough become unconscious,” says Clement. The treatment is to get some sugar in you, fast—people with diabetes might carry glucose tablets, but if those aren’t available drink a cup of juice, Clement says.

Super-high blood sugar is also dangerous
The other blood sugar extreme is high blood sugar, or hyperglycemia. “Hyperglycemia happens when excessive amounts of glucose are in the bloodstream, typically as a result of [a person with diabetes] consuming too many carbohydrates, which convert into glucose in the blood,” Palinski-Wade says. “This can lead to fatigue, excess thirst, and excessive urination. If blood glucose levels climb to extremely high levels, the risk of loss of consciousness, coma, and even death are possible.” This is another reason that people with diabetes need to consume the right portions of carbs throughout the entire day, or take enough insulin to process the food they are eating. (Here’s more on the difference between hyperglycemia and hypoglycemia.)
A complex mix of factors can affect blood sugar in people with diabetes. Stress or an infection can make it harder for medication to control blood sugar; exercise can lower blood sugar (in a good way), and consuming carbs with fat, protein, or fiber can also slow down digestion of carbohydrates and reduce the blood sugar impact on the body.
It’s rare for there to be symptoms of very high blood sugar in people without diabetes. In those cases, it might be triggered by serious illnesses, some medications, stomach surgery, or low levels of certain hormones, reports the Hormone Health Network.

Type 1 and type 2 diabetes are very different conditions
Learning about the different types of diabetes—there are several ways glucose can be mismanaged by the body—can be an important preventive strategy. Type 2 diabetes, in which your body develops insulin resistance, is the most common type of diabetes and often develops later in life (although children can get it too). Genetics and lifestyle play a role in type 2 diabetes, which can sometimes be delayed or prevented by sticking to a healthy lifestyle, including regular exercise, and avoiding weight gain. Type 1 diabetes, however, can not be prevented with lifestyle choices. Type 1 diabetes occurs when the pancreas stops making insulin due to an autoimmune attack; it can be diagnosed in children and young adults and is sometimes called “juvenile diabetes.” (These surprising habits can lead to type 2 diabetes.)

Illness or stress can affect your glucose level
One way stress could be making you sick is by increasing the chance that blood sugar will rise. “Stress and illness causes high blood glucose levels because during these times, your liver releases extra glucose to ensure enough energy is readily available,” Zuckerbrot says. “At the same time, cortisol and growth hormone are released which makes your body less sensitive to insulin. As a result, blood glucose levels are higher than usual.” But it’s not irreversible: Research in Diabetology & Metabolic Syndrome found that people with diabetes were able to reduce their glucose levels after stress management training with a psychologist where patients learned muscle relaxation techniques, among others.

Inactivity also negatively affects blood sugar
As if you needed more science-backed reasons to exercise, here’s another: You can help regulate your glucose levels and reduce your risk of prediabetes and type 2 diabetes with exercise. Why is inactivity linked to higher blood sugar? “Inactivity leads to a decrease in your insulin sensitivity and increases your insulin requirements,” says Zuckerbrot. Exercise uses up your body’s glucose, making you more sensitive to insulin. According to the American Diabetes Association, physical activity can lower your blood glucose for up to 24 hours or more after you work out, and regular exercise can lower your overall blood glucose level (A1C). On the other hand, research published in the Journals of Gerontology found that two weeks of inactivity could increase the risk of blood sugar-control problems in older, overweight people who already had prediabetes.

HIIT training, specifically, could help glucose
High-intensity interval training (HIIT) is one of the best anti-aging workouts and one of the ways it may increase your longevity is by lowering glucose levels. “Researchers at the University of Turku, Finland, studied how high-intensity interval training alters the brain’s glucose metabolism in physically inactive insulin-resistant people,” Zuckerbrot says. “Only two weeks of HIIT training reduced glucose metabolism in all areas of the brain.” An earlier study by the same researchers found that HIIT increased glucose metabolism in muscles as well. Because the brain runs on glucose, this workout could benefit your mind as well as your body.

Belly fat is particularly bad for blood sugar
Research has found that having excess fat on the body can impact the risk of diseases like type 2 diabetes, and where it’s located on the body can matter too. Visceral fat—the type of fat that pads organs in the abdomen—puts you at a higher risk of type 2 diabetes, according to a 2018 study in Nature Genetics. Belly fat (which can be either visceral or subcutaneous fat, or fat underneath the skin) is known to promote inflammation and increase the risk of insulin resistance. And another study from Massachusetts General Hospital found that it’s not just an association—there are actually genetic variants associated with an apple shape-body (carrying weight around the midsection rather than the arms or legs) that predisposes a person to type 2 diabetes. But the good news is, according to the American Diabetes Association, that even losing 10 to 15 pounds can make a big difference in your ability to control blood sugar.

Blood sugar tests are important
So, should you get your blood sugar levels checked? It will likely depend on your age and risk factors. The American Diabetes Association suggests asymptomatic people get tested at a minimum every three years over age 45. But, because high blood sugar is “often asymptomatic and can cause complications if left untreated, people with risk factors such as being overweight, having a high-risk race or ethnicity [such as African-American], or lipid problems should be screened periodically with a blood test,” says endocrinologist Kathleen Dungan, MD, of The Ohio State University Wexner Medical Center. In addition, “anyone with a family history of diabetes should get their glucose tested and inquire about having your A1C checked as part of their annual visit to their primary care physician,” Clement says. If you have risk factors, talk to you doctor about how often you should be screened and what age to start.
If you’re pregnant, a doctor will also have you take a glucose tolerance test, which involves drinking a sugary liquid to see how your body responds. It’s a test that can pick up gestational diabetes. “During pregnancy, women’s bodies have to produce three times more insulin than normal,” Clement says. “Not everyone can handle this increased demand, and for those women, blood sugar starts going up around the 23rd or 24th week of pregnancy. These women likely will be placed on a special diet to control blood sugar.”

You should tell your doctor about these symptoms
If you have any of the signs of high blood sugar, you should definitely let your doctor know. If you’re constantly thirsty, have frequent urination, and are extremely tired, that could point to a blood sugar issue. You should bring your concerns to your doctor especially if you have additional risk factors like being overweight, not exercising, and having a family history of diabetes. But because more than 84 percent of people with prediabetes don’t know they have it according to the CDC, the best strategy is to take steps to prevent the condition and get tested, particularly if you are at higher risk of type 2 diabetes.

Cinnamon may improve your glucose level
Besides flavoring food, cinnamon might have potential health benefits. “Some research indicates cinnamon may improve insulin sensitivity,” Palinski-Wade says. “For those with insulin resistance, this may help the body to process glucose more easily, resulting in less of a rise in blood glucose levels.”

Food order may impact glucose levels
Among the sneaky things that raise your blood sugar levels may be the order in which you eat foods during any given meal. Research from Weill Cornell Medical College tested what happened when participants ate the same meal on different days. First they ate carbs, followed by protein, vegetables, and fat; another day they ate the protein, veggies, and fat first, followed by the carbs. Both glucose and insulin were lower when they ate the carbs last. Palinski-Wade says eating the carbs after the other foods may slightly reduce the time it takes to convert the carbs into glucose, preventing a spike after a meal.

Glucose levels may be linked to dementia and Alzheimer’s
There may be more kinds of diabetes than we know, such as type 3c, which occurs after pancreatitis. But there’s yet another type that researchers have been exploring. “Researchers are looking at how sugar affects the brain—specifically, some are referring to Alzheimer’s disease as type 3 diabetes because of this research,” Clement says. This isn’t exactly surprising given the brain’s reliance on glucose for proper functioning. In addition, diabetes can damage blood vessels, which can prevent your brain from getting the blood flow it needs. One study of over 2,000 participants found that glucose levels in those who went on to develop dementia were elevated—even among people without diabetes. The findings suggest high blood sugar could be a risk factor for dementia.

Mindfulness may reduce glucose levels
Mindfulness may help your blood sugar level. In a 2016 study from Brown University, participants with high scores for mindfulness, which they defined as being aware of your present thoughts and feelings, were more likely to have healthy glucose levels than people with low scores. The researchers surmised that although it’s only an association, not a cause and effect, mindful people were more likely to self-motivate themselves to exercise and eat right, and to resist cravings. According to study author Eric Loucks, this was the first study to look at the connection between diabetes and mindfulness, which may be a new way to reduce your risk. Try starting your morning with these mindfulness exercises.

Artificial sweeteners don’t benefit blood sugar—or do they?
There’s mixed reviews about the impact of artificial sweeteners on blood sugar level. Some research has suggested that the sweet taste is enough to trick your body’s response, as if it was actually receiving sugar. But, the sweetener stevia may hold some promise for actually reducing blood sugar, according to one study. “Some research suggests stevia may have a beneficial impact on blood glucose levels, however, more research needs to be done in this area,” Palinski-Wade says.

Poor sleep isn’t great for blood sugar
Fact: You are more likely to eat more when you’re sleep deprived. Plus, you’ll likely be craving junk food, which is not exactly great for your blood sugar level. According to the National Sleep Foundation, the connection may be because with lack of sleep, hormones get out of whack, and the stress hormone cortisol may prevent insulin from doing its job properly. With short-term sleep deprivation, levels can go back to normal with two nights of good sleep. But for long-term problems sleeping, including sleep apnea, see your doctor to reduce your diabetes risk.
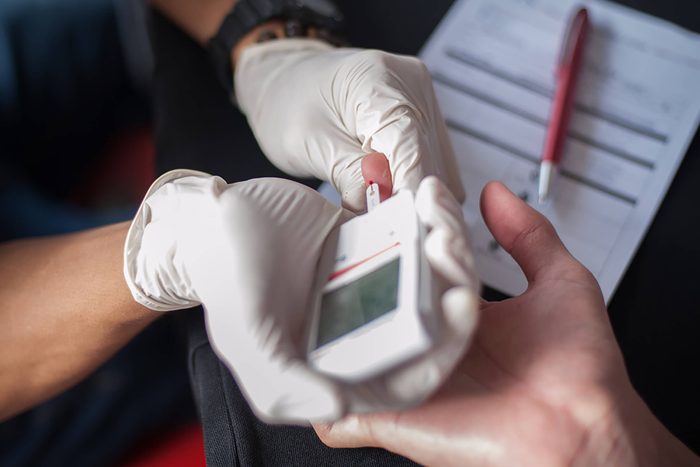
There are several ways to self-test blood sugar
One of the most important tests people with diabetes use is the daily finger prick, in which a drop of blood is placed on a test strip and inserted into a blood sugar meter to quickly get a blood sugar reading. People with diabetes often need to self-test their blood sugar (particularly if they are on insulin) to make sure it’s steady. However, there are other ways to self-test blood sugar, including continuous glucose monitors. More often used by people with type 1 diabetes, the devices use a small sensor wire that is inserted below the skin’s surface to continuously monitor glucose levels. The sensors need to be replaced every three to seven days, and people who use them typically still need to do finger-prick tests to make sure the devices are working correctly.

Get educated about diabetes management
There are science-backed strategies to drop blood sugar back to a normal range, and Clement says she puts diabetes education at the forefront of what everyone should know about glucose. “There is not enough emphasis on the consequences of uncontrolled diabetes and resulting complications such as neuropathy, heart disease, eye disease, and kidney disease,” she says. “In addition to good medical care, diabetes self-management education can help patients learn to take care of their disease.”

